8 Tips to Help with Recovery from Shoulder Surgery
Shoulder surgery can be a daunting experience and the day to day can be quite challenging post-surgery. However, in addition to following the essential instructions provided by your doctor to ensure a full and proper recovery, being ready at home can dramatically help reduce any anxiousness and make the process more comfortable.
Below are eight at-home success tips to help you to prepare and make the most out of your recovery from shoulder surgery.
1. Follow Your Doctor’s Instructions
After surgery, your doctor will provide you with detailed instructions on how to care for your shoulder. It’s essential to follow these instructions to ensure that you recover as quickly as possible. Some of the instructions may include initial physical therapy exercises, pain medication recommendations, and keeping your shoulder immobilized with a properly fitted sling. Instructions vary per procedure so be sure to diligently read through all information provided to you.
2. Consider Which Arm Your Surgery Will Be On
If surgery is taking place on your dominant arm, you’ll want to prepare by practicing daily tasks with your non-dominant arm.
As most people do not practice being ambidextrous, everyday tasks such as brushing your teeth, going to the bathroom, drinking from a cup, eating, opening doors, etc. all may be a learning curve for the first few weeks. Practicing these types of tasks prior to surgery may help ease this learning curve once surgery has taken place.
3. Prepare to Get Dressed and Do Your Hair
Throughout the first few weeks after surgery, you may not be able to:
- lift your arm above your head
- lift your arm out in front of you
- lift your arm out to the side of you
To help with this, loose-fitting shirts, button-downs, and zip-ups are highly recommended for use after surgery. There are post-surgical shirts available at various online retailers if that’s an option you’d like to use as well.
It’s also recommended to practice doing your hair with one hand for those who may need to do this independently post-surgery. If you do a google search for “how to put hair in a ponytail with one hand” or something similar, you will find many tutorials to help get the hang of these tasks.
4. Build Your At-home Recovery Supply
Many patients find having little everyday items (such as those listed below) can make a big difference during shoulder surgery recovery. So you don’t have to worry about venturing out soon after surgery, it is recommended to stock up on a few weeks’ worth of food and toiletries as well.
- Long-handled back scrubber
- Detachable shower head
- Shower chair
- Frozen meals
- Multiple button-down shirts, front closure bras, zip-up sweaters or hoodies, oversized t-shirts, looser fitting pants
- Pillow wedge
5. Get Plenty of Rest and Reduce Stress
Getting plenty of rest is crucial to a successful recovery. Your body needs time to heal, and rest is the best way to facilitate that process. It’s normal to experience fatigue after surgery, so be sure you rest whenever you feel tired. Sleeping in a recliner or propping yourself up with multiple pillows can help reduce pain and inflammation.
Additionally, it’s important to reduce your stress throughout recovery. Dialing back on your daily responsibilities should be a priority. Prepare those who are typically dependent upon you so they are ready when the time comes, and you can truly optimize your recovery.
6. Focus on Nutrition and Hydration
Following a whole food nutrition plan is essential for recovery from surgery. Be sure to eat a well-balanced diet that includes:
- plenty of fruits and vegetables
- lean proteins
- whole grains
This will ensure you’re receiving all the essential vitamins and minerals necessary for proper healing.
Hydration is also a very large component of ensuring a full recovery. Approximately 60% of our bodies are composed of water. Consuming enough water helps to avoid any potential complications such as infections and helps to boost the immune system that is typically weakened after surgery. The US National Academies of Sciences, Engineering and Medicine recommends adults consume between 92oz – 124oz of water per day. This equates to about 3-4 32oz bottles throughout the day.
7. Take It Slow and Be Patient
Recovery takes time, and you shouldn’t rush the process. Remember that taking it slow doesn’t mean you can’t do anything; it simply means for the first few weeks you’ll want to opt for light activities or adventures. With doctor guided permission, you can gradually increase the intensity of everyday activities. Remember to avoid any activities that put pressure on your shoulder, don’t lift anything heavy until your doctor gives you the go-ahead, and ask your loved ones for help when necessary.
8. Handling Setbacks
Throughout your recovery journey, you may experience setbacks. This is normal and you shouldn’t get discouraged. A few tricks that have helped many patients push through recovery are:
- Keeping a positive attitude and focusing on your recovery goals.
- Celebrate small victories, like being able to move your arm a little more each day.
- Remember, your body is healing, and it will take time.
- Embrace this period of more down time than you’re used to, and remember recovery is temporary. You’ll be back to doing the things you love to do soon.
We understand the process of recovering from shoulder surgery is not easy. It requires patience, perseverance, and following your doctor’s instructions to a T. As mentioned, it is temporary and ultimately will be the vehicle to get you back to living pain free. Prepare ahead of time, get plenty of rest, focus on your nutrition and hydration, and you’ll be back to the swing of things.
At Colorado Springs Orthopaedic Group, our teams are always here for you whenever you need us throughout your recovery journey. If you have any questions or concerns, simply send a message to your surgical team through your patient portal or give us a call at 719-632-7669. We’ll be back in contact with you as soon as possible.
Meet Our Sports Medicine Providers

Jamie Friedman, MD

Michael Huang, MD

Christopher Jones, MD

John Redfern, MD

Richard Stockelman, MD

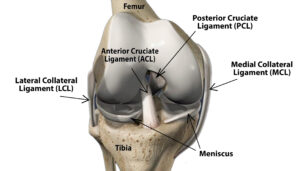 ne to bone and provide stability within the joint.
ne to bone and provide stability within the joint.



















 The exact reason positive thinkers tend to have better surgical healing outcomes is still not completely understood. Scientists do however, have a few theories to explain the benefit of positive thinking:
The exact reason positive thinkers tend to have better surgical healing outcomes is still not completely understood. Scientists do however, have a few theories to explain the benefit of positive thinking:
 Protective gear is the first line of defense in preventing injury for kids playing sports. Of course that gear will be different depending on what sport your child plays. Protective gear may include:
Protective gear is the first line of defense in preventing injury for kids playing sports. Of course that gear will be different depending on what sport your child plays. Protective gear may include:
 Your daily routine may feel like it’s controlling you. It’s the long list of tasks you must complete every day from getting the kids to school, to going to work, then making dinner and getting everyone to bed. If you are mindful about the simple steps in this process, you can turn your routine into a ritual that you control. When you create daily rituals, you allow the small steps in your day to take on greater significance. This can add happiness and meaning to your daily life.
Your daily routine may feel like it’s controlling you. It’s the long list of tasks you must complete every day from getting the kids to school, to going to work, then making dinner and getting everyone to bed. If you are mindful about the simple steps in this process, you can turn your routine into a ritual that you control. When you create daily rituals, you allow the small steps in your day to take on greater significance. This can add happiness and meaning to your daily life.
 Bicycles are considered vehicles in most states, and rules apply for safely operating bikes in the same way they do to cars. In order to avoid accidents or injuries follow these tips.
Bicycles are considered vehicles in most states, and rules apply for safely operating bikes in the same way they do to cars. In order to avoid accidents or injuries follow these tips. Weight gain: more time in front of a screen translates into less physical activity
Weight gain: more time in front of a screen translates into less physical activity Choosing a Marathon. One of the first things you will have to decide is which marathon you would like to participate in. Some important things to consider are:
Choosing a Marathon. One of the first things you will have to decide is which marathon you would like to participate in. Some important things to consider are: Do you have hip pain when you are active? Does the pain lessen when you rest?
Do you have hip pain when you are active? Does the pain lessen when you rest? When you first start lifting, you’re better off having slightly too little weight rather than too much. Experiment when doing your workout and see what weight size feels comfortable. It should be somewhat difficult to complete the last few reps of your final set of lifts. Your arms or legs may shake with the effort, but you should not feel sharp pain.
When you first start lifting, you’re better off having slightly too little weight rather than too much. Experiment when doing your workout and see what weight size feels comfortable. It should be somewhat difficult to complete the last few reps of your final set of lifts. Your arms or legs may shake with the effort, but you should not feel sharp pain. A military career is a rewarding one that may bring with it different injuries and chronic conditions. From jumping out of planes to running with heavy packs, the life of a serviceman or servicewoman is hard on a body. At
A military career is a rewarding one that may bring with it different injuries and chronic conditions. From jumping out of planes to running with heavy packs, the life of a serviceman or servicewoman is hard on a body. At 
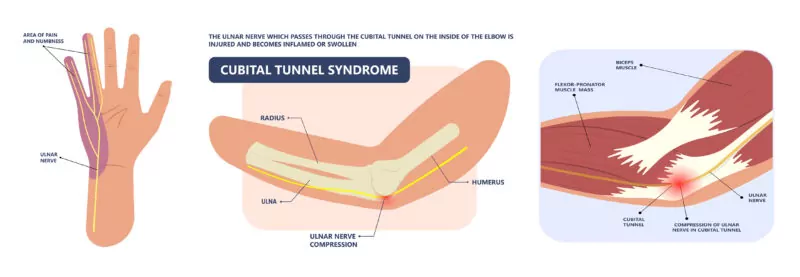
 Most of the positions you can hold your phone in are not good for your muscles. This is why developing smartphone hand pain is so common in today’s times. When using your phone, try to keep your wrist straight as much as possible. You can do this by texting with once hand rather than using both thumbs. Another method would be setting your phone on a flat surface while you type.
Most of the positions you can hold your phone in are not good for your muscles. This is why developing smartphone hand pain is so common in today’s times. When using your phone, try to keep your wrist straight as much as possible. You can do this by texting with once hand rather than using both thumbs. Another method would be setting your phone on a flat surface while you type.
 Whether you have an Apple Watch or some other variety of smart watch, this piece of wearable technology can help with physical therapy tracking and goals. Some fitness features included in a smart watch might be:
Whether you have an Apple Watch or some other variety of smart watch, this piece of wearable technology can help with physical therapy tracking and goals. Some fitness features included in a smart watch might be: Many conditions can lead to chronic shoulder pain including:
Many conditions can lead to chronic shoulder pain including: Dr. Roger Sung
Dr. Roger Sung It’s very common to experience a sore ankle when you get back into running, jogging, biking, or other fitness routines. Your ankles take a lot of the force when you are doing physical activity. The soreness you experience may be from stress on the joint, ligaments, tendons, or muscles. A few simple steps can prevent a sore ankle.
It’s very common to experience a sore ankle when you get back into running, jogging, biking, or other fitness routines. Your ankles take a lot of the force when you are doing physical activity. The soreness you experience may be from stress on the joint, ligaments, tendons, or muscles. A few simple steps can prevent a sore ankle. Will you be able to make your daughter’s wedding the summer after your surgery? Questions like this may weigh on your mind as you schedule your knee replacement. Air travel poses some unique challenges. It often involves lots of walking to and from your gate, sitting in a small seat for several hours, and the added concern of developing a blood clot. Here are some precautions you can take to have a safe and comfortable flight:
Will you be able to make your daughter’s wedding the summer after your surgery? Questions like this may weigh on your mind as you schedule your knee replacement. Air travel poses some unique challenges. It often involves lots of walking to and from your gate, sitting in a small seat for several hours, and the added concern of developing a blood clot. Here are some precautions you can take to have a safe and comfortable flight: A Flexible Spending Account, or FSA, lets you set aside money for medical expenses. Since your employer removes the funds from your paycheck before taxes, you realize the tax savings. You and your employer can add money to the account up to the limits outlined by the IRS. It is important to note that the money in a Flexible Spending Account must be used by the end of the year, otherwise your employer can keep the unused funds. Some employers may let you to pay expenses for the previous two months or roll over $500 to the next year. Each year you must re-enroll in the FSA program. You will also need to:
A Flexible Spending Account, or FSA, lets you set aside money for medical expenses. Since your employer removes the funds from your paycheck before taxes, you realize the tax savings. You and your employer can add money to the account up to the limits outlined by the IRS. It is important to note that the money in a Flexible Spending Account must be used by the end of the year, otherwise your employer can keep the unused funds. Some employers may let you to pay expenses for the previous two months or roll over $500 to the next year. Each year you must re-enroll in the FSA program. You will also need to:






 will receive the highest quality of outpatient care and friendly, attentive service. The
will receive the highest quality of outpatient care and friendly, attentive service. The 
















 shoulder replacement. Each year over 53,000 people have shoulder replacement surgery. This procedure relieves pain effectively. In shoulder replacement surgery, the surgeon removes the damaged parts of the shoulder and prosthetic parts are put in to restore the joint.
shoulder replacement. Each year over 53,000 people have shoulder replacement surgery. This procedure relieves pain effectively. In shoulder replacement surgery, the surgeon removes the damaged parts of the shoulder and prosthetic parts are put in to restore the joint.





 Summertime and broken bones may not seem to be two things that go together. Unfortunately, this is not the case. With the increase in outdoor activities, bone fractures are among the most common summertime injuries, especially in children.
Summertime and broken bones may not seem to be two things that go together. Unfortunately, this is not the case. With the increase in outdoor activities, bone fractures are among the most common summertime injuries, especially in children.


 It is time to seek professional help. Depending on the severity of the sprain you may be on crutches for a few days or put into a boot or a splint to restrain the movement of your ankle. After the resting period is over, you may be referred to a physical therapist for specific exercises to rehabilitate your ankle.
It is time to seek professional help. Depending on the severity of the sprain you may be on crutches for a few days or put into a boot or a splint to restrain the movement of your ankle. After the resting period is over, you may be referred to a physical therapist for specific exercises to rehabilitate your ankle.

 ACL Reconstruction
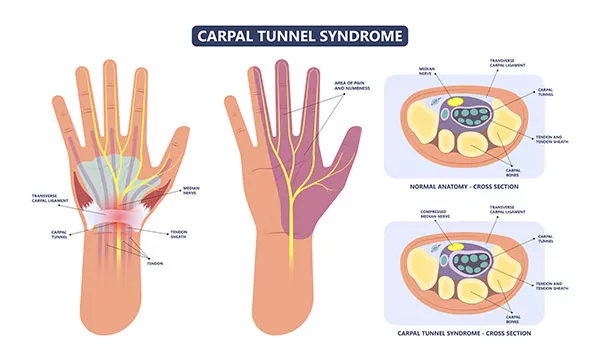
ACL Reconstruction What can prevent carpal tunnel syndrome?
What can prevent carpal tunnel syndrome?




 normally smooth cartilage in the shoulder joint disappears, this creates a bone-on-bone situation causing significant pain while also limiting movement. Shoulder replacement surgery is advised when:
normally smooth cartilage in the shoulder joint disappears, this creates a bone-on-bone situation causing significant pain while also limiting movement. Shoulder replacement surgery is advised when: Alternately, with a fractured finger you may experience:
Alternately, with a fractured finger you may experience:
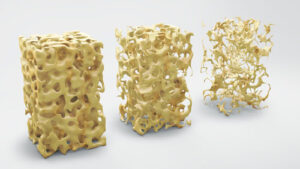 Osteopenia, Osteoporosis, and Osteonecrosis are often called silent diseases because they have so few symptoms, but complications can cause disability, pain, and sometimes death. These diseases of the bone occur when people lose too much bone mass, make too little new bone tissue, or both. Up to 54 million Americans suffer from osteoporosis or osteopenia (low bone mass) which increases the risk of osteoporosis. Another disease, osteonecrosis, is caused by low blood flow to the bone.
Osteopenia, Osteoporosis, and Osteonecrosis are often called silent diseases because they have so few symptoms, but complications can cause disability, pain, and sometimes death. These diseases of the bone occur when people lose too much bone mass, make too little new bone tissue, or both. Up to 54 million Americans suffer from osteoporosis or osteopenia (low bone mass) which increases the risk of osteoporosis. Another disease, osteonecrosis, is caused by low blood flow to the bone.
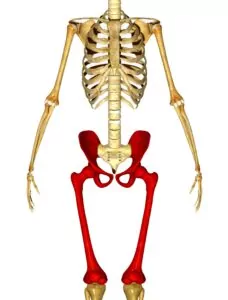 Anterior hip replacement is a minimally invasive option for hip replacement surgery when compared to the posterior procedure. Even though this is not a new procedure, it is estimated that only 15%-20% of all hip replacements use this unique approach. Anterior (front of the joint) hip replacement surgery is done with more specialized instruments and through smaller incisions. This provides several advantages over the posterior procedure. First, this is a muscle splitting approach rather than a muscle cutting approach. The surgery is performed between a natural separation of the muscles. This allows the integrity of the hip muscles to stay in place in order to better support the newly reconstructed hip joint. Second, with anterior hip replacement there is less post-surgical pain, faster healing time, and a shorter hospital stay. The final benefit of anterior hip replacement is the decreased risk of dislocations. Since the muscles were not cut, there is less healing involved. After the healing process is complete, the patient will enjoy a better range of motion as well.
Anterior hip replacement is a minimally invasive option for hip replacement surgery when compared to the posterior procedure. Even though this is not a new procedure, it is estimated that only 15%-20% of all hip replacements use this unique approach. Anterior (front of the joint) hip replacement surgery is done with more specialized instruments and through smaller incisions. This provides several advantages over the posterior procedure. First, this is a muscle splitting approach rather than a muscle cutting approach. The surgery is performed between a natural separation of the muscles. This allows the integrity of the hip muscles to stay in place in order to better support the newly reconstructed hip joint. Second, with anterior hip replacement there is less post-surgical pain, faster healing time, and a shorter hospital stay. The final benefit of anterior hip replacement is the decreased risk of dislocations. Since the muscles were not cut, there is less healing involved. After the healing process is complete, the patient will enjoy a better range of motion as well. With basketball, as well as all sports, prevention of injury is key. To prevent foot and ankle injuries, the player needs the right kind of foot support. A good quality basketball shoe as well as taping up your ankle before a game can go a long way for staying on the court. To prevent hip and thigh injuries, do some good stretching and warming up before the start of every game and practice. For your knees, the best
With basketball, as well as all sports, prevention of injury is key. To prevent foot and ankle injuries, the player needs the right kind of foot support. A good quality basketball shoe as well as taping up your ankle before a game can go a long way for staying on the court. To prevent hip and thigh injuries, do some good stretching and warming up before the start of every game and practice. For your knees, the best 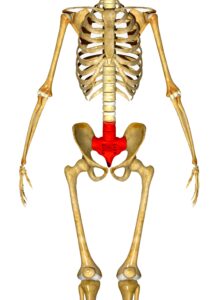 Function and Causes
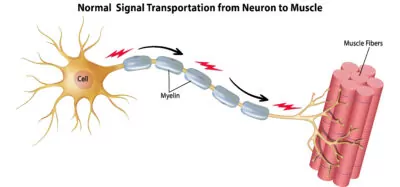
Function and Causes Stem cells are the cells of the body that are undifferentiated, meaning they can turn into other cell types. Stem cells can be obtained from the umbilical cord, bone marrow, or adipose (fat) tissue. The stem cells obtained from the embryonic environment are preferred to other types of stem cells, first because the potential of stem cells is thought to decrease with age and second because it can be painful to extract bone marrow.
Stem cells are the cells of the body that are undifferentiated, meaning they can turn into other cell types. Stem cells can be obtained from the umbilical cord, bone marrow, or adipose (fat) tissue. The stem cells obtained from the embryonic environment are preferred to other types of stem cells, first because the potential of stem cells is thought to decrease with age and second because it can be painful to extract bone marrow.
