Cubital Tunnel Syndrome
Terms to know:
- Physiologic effect: activities that affect body movement without any relation to a specific disease.
- Physiologic cascade: sequence of repeated activation reactions due to a series of developments from a specific initial stimulus – example: compressing a nerve can cause muscles to involuntarily spasm due to a lack of blood flow and neurological control over the signal sent to the muscles in which that specific nerve controls.
- Sensory Nerve Fibers: transmit sensations, such as temperatures and pain, to the brain and spinal cord. These fibers control the sensations you feel on your skin or within your body.
- Peripheral Motor Nerve Fibers: transmit signals from the brain and spinal cord to muscles. These fibers tell your body how to move and function.
- Vascularized Fat Flaps: fatty tissue that has blood vessels capable of delivering nutrients to cells within the tissue.
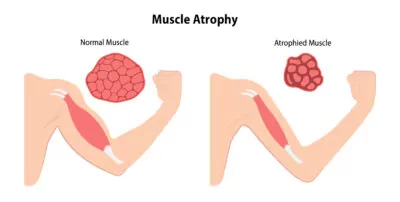
- Muscle Atrophy: muscle weakness or loss of muscle mass
What is Cubital Tunnel Syndrome?
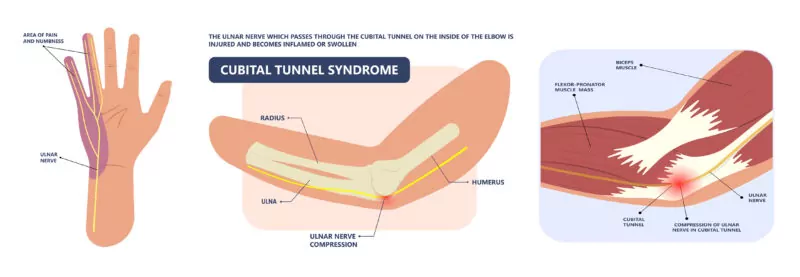
“Cubital tunnel syndrome” is a collection of symptoms of the upper limb caused by increased pressure within or on the ulnar nerve as it passes along the backside or inside aspect of the elbow. This is indicated within the illustrations below. It is one of many “compressive neuropathies” in which our nerves contribute to symptoms of pain, numbness, and/or motor dysfunction. These symptoms occur from a physiologic cascade of breakdown within the nerve triggered by reduced blood flow to the lower arm.
A way to demonstrate this physiologic breakdown is to take your finger and press on your skin. You’ll notice, your skin will temporarily turn white as pressure is applied due to the lack of blood flow to that specific area. The same thing happens with our nerves when there is external pressure applied to a nerve that reduces the local blood flow into the area. This can also occur when there is internal pressure within the nerve. Nerves typically display a surge of dysfunction symptoms that are initially temporary but can lead to irreversible long-term changes if not addressed.
Nerve Compression
For those interested in this sequence of breakdown and dysfunction, nerve compression in short produces diminished local blood flow from pressure placed on the compressed area. Reference back to pressing your finger on your skin for any amount of time. This reduction of local blood flow then creates altered signals to your brain. Similarly, consider the times your foot falls asleep when one leg is crossed over the other. This painful tingling and perhaps muscle clumsiness, is rapidly reversed when you simply change the position and “shake it out”. In other words, when you restore local blood flow.
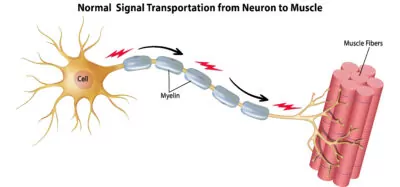
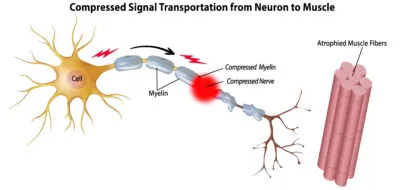
However, over time chronic nerve compression leads to swelling within the nerve. This results in an alteration of the protein transport sequence necessary for proper nerve fiber function along the length of the nerve. See the illustrations below. In addition, compression on the “insulation” (called Myelin) around our peripheral nerves that promotes faster conduction, reduces the ability for nerve fibers to transmit a signal to the muscle to operate. After prolonged periods, this can lead to muscle atrophy.
Nerve Breakdown and Dysfunction
Sensory nerve fibers tend to display breakdown and dysfunction first, with motor nerve fibers secondarily. Eventually, with prolonged compression, the normal connective tissue around the nerve fibers becomes thick and scarred resulting in reduced capacity of the fibers themselves. Once this occurs, there is potential that these fibers may not recover full function, even if the nerve is later decompressed through surgical intervention.
Unfortunately, although this sequence has been well defined in animal studies, it is difficult to predict the timing of this deterioration in humans. There are several variables that may contribute to either the resiliency or vulnerability of individual patients to progress to the endpoint of permanent nerve fiber scarring and dysfunction. Because of this, if you are experiencing ongoing symptoms of any form of nerve compression, it’s recommended to be seen by an orthopedic specialist.
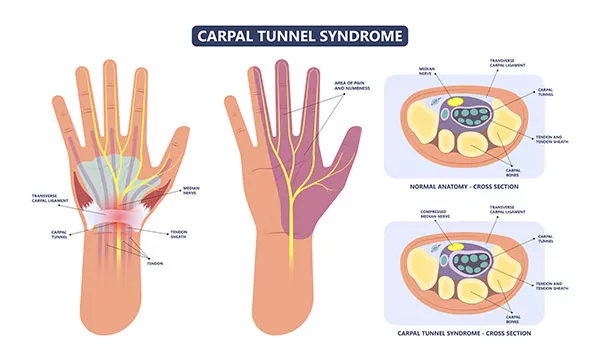
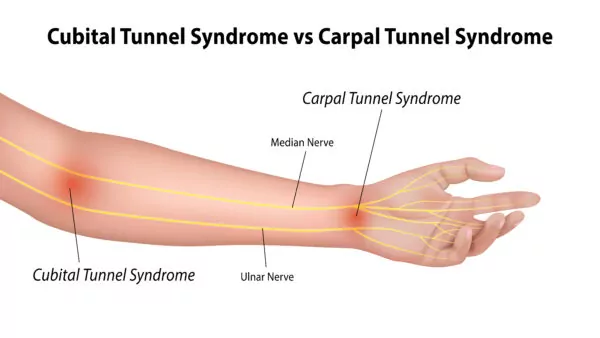
Carpal Tunnel Syndrome vs Cubital Tunnel Syndrome
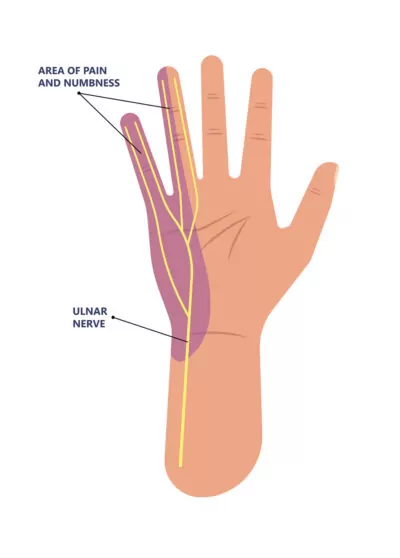
The well-known Carpal tunnel syndrome is the most common compressive neuropathy in the upper extremity and involves compression of the median nerve at the wrist. Alternatively, Cubital tunnel syndrome, as discussed here, is slightly less frequent and results from compression of the ulnar nerve as it travels along the inside of the elbow. We have normal structures that surround and support the location of the ulnar nerve as it travels behind the medial epicondyle. The medial epicondyle is that bony prominence on the inside of your elbow. However, with cubital tunnel syndrome, these normal structures, along with a normal increase of tension along the ulnar nerve as the elbow bends, can create diminished local blood flow and initiate the breakdown and dysfunction cascade mentioned above.
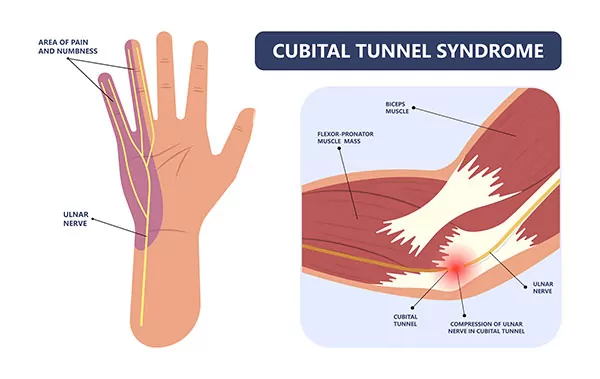
The symptoms resulting from this breakdown are usually quite easily recognizable. Patients usually complain of:
- Numbness along the ulnar border of the hand (ring and small finger)
- Tenderness along the inside portion of the elbow
- Clumsiness and weakness in the hand
Many patients will experience the symptoms of numbness along the side of the hand and elbow pain during the night, as most of us sleep with our elbows bent. Symptoms may also occur with similar positions during the day. These can be activities such as talking on the phone, typing, leaning on a surface, or vigorous pushing and pulling. Most patients will notice numbness, typically around the inside of the elbow first. Clumsiness may emerge later. Over time, with chronic compression, the numbness will persist around the clock and patients will exhibit actual atrophy of the smaller muscles within the hand. When addressed soon enough, we can aim to stop the process before it reaches this stage.
Some patients can have these problems secondary to instability of the ulnar nerve. You’ll notice when the nerve is instable, it will snap back and forth over the bony prominence on the inside of the elbow whenever flexing or extending the arm.
Cubital Tunnel Syndrome Treatment
It is important to note that not all patients will manifest these exact symptoms. There are obviously variant presentations that require your physician to be attentive to symptoms and additional examination findings. Let’s discuss the process of what goes into the diagnosis of Cubital Tunnel Syndrome and the various treatment methods available.
Diagnosis
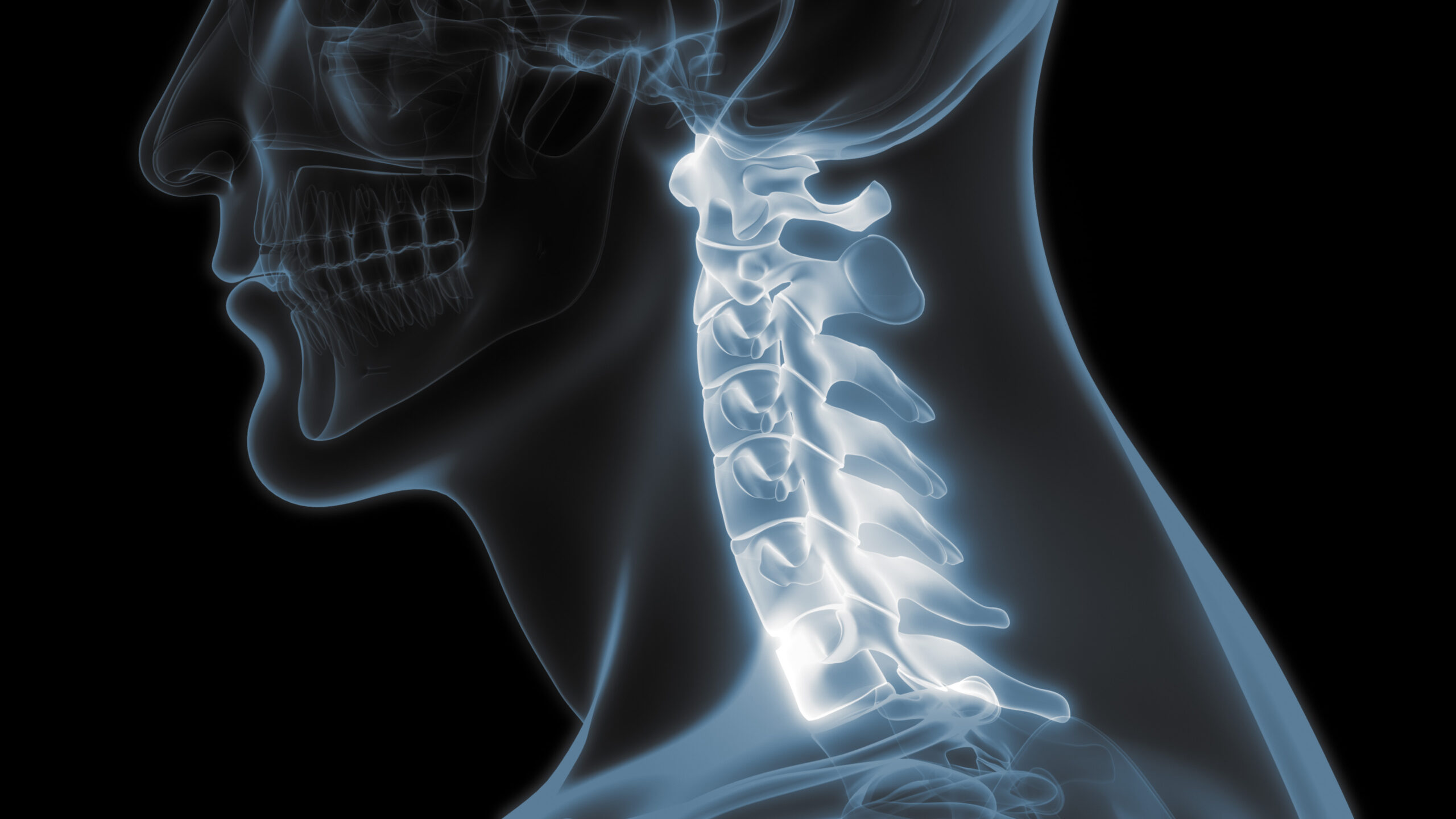
Aside from taking your injury history and listening to your symptom patterns, your clinician will perform a physical exam. This exam will include isolating the level of the injury to the nerve, the degree of nerve dysfunction, and other contributing factors. Consider that these symptoms may also be manifestations of compression of a cervical nerve root in the neck, compression of a group of nerves passing underneath your clavicle. This condition is specifically referred to as Thoracic Outlet Syndrome.
Additionally, compression elsewhere along the ulnar nerve within the arm, or compression of the ulnar nerve within the wrist, could be potential causes for your symptoms. Furthermore, sometimes symptoms of hand clumsiness or muscle atrophy is a manifestation of peripheral neuropathy, an intrinsic disease of the nerves themselves, independent of compression. Diabetic neuropathy is one form of this potential cause.
To help distinguish your diagnosis, your physician may also employ electrodiagnostic studies (often referred to as an “EMG”). These EMG’s are performed by an outside provider to help “map out” locations and severity of your nerve compression. From here, your physician will work with you to build a treatment plan suitable for your individual needs.
Initial Treatment
Initial treatment for patients with early symptoms and findings, involves avoiding compression and traction (pulling) on the ulnar nerve. For example, you will want to avoid leaning on your elbow or activities such as heavy weightlifting where weight is pulling on the affected arm.
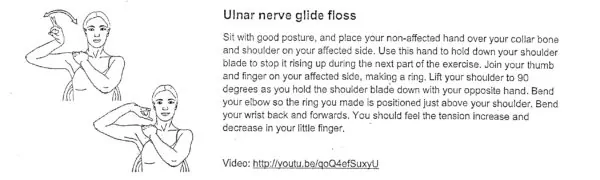
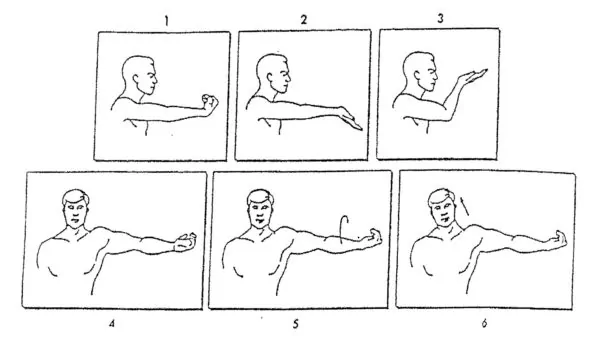
The simplest initial treatment for pain relief is to use a nighttime splint to block hyperflexion of the elbow. Hyperflexion while sleeping is often the main contributor of symptoms for patients with this problem. For many patients, “Nerve glide” exercises such as the below, may also be helpful. There may, however, be some patients who do not respond to these exercises.
This condition, in its earliest form, is often reversible and over 50% of patients do not require surgery. Improvement in symptoms may be gradual and take a few months.
Cubital Tunnel Syndrome Surgery
If symptoms persist or if you exhibit more advanced phases of nerve compression, your physician may recommend surgical treatment to decompress the nerve and enhance blood flow. The most basic surgical measure is “decompression” of the ulnar nerve as it passes through the cubital tunnel. Sometimes, this is enough, allowing the nerve more mobility with less local compression as it glides through the cubital tunnel. However, this procedure may not be effective for every case.
The most common procedure performed is the decompressing of the nerve followed by “transposition” of the nerve to the front of the elbow, just anterior to the medial bony prominence. With this maneuver, the nerve is both decompressed and placed in a position where it is no longer subjected to stretching or tension. In some cases, the nerve may be left lying just superficial to the muscle on the inside of the elbow. Alternatively, the nerve can also be buried within that musculature to further decrease tension.
Whatever the procedural method selected, the nerve needs to glide freely with minimal tension or kinking around anatomic structures.
Cubital Tunnel Surgery Recovery
Our physicians rarely immobilize, or restrain, the elbow following ulnar nerve decompression or transposition surgery. This is because we want your nerve to glide freely and limit potential for scarring. However, we do not want any form of violent pushing, pulling, or twisting over the initial 4-to-6-week window. To provide protection against these violent movements, we will prescribe for your surgical dressings to be in place for the initial 7 days. After those 7 days, you will typically be able to remove the dressing and allow running water (faucet or shower) over your wound. We usually have patients return for a follow up visit within 10-to-14-days post operation to complete a wound check and suture removal.
Most patients do not require formal physical or occupational supervised therapy after cubital tunnel syndrome surgery. However, we may provide instructions for simple exercises that you can perform independently at home. If further supervised visits are needed, our occupational therapists are certainly available to accommodate as such.
Things to Know Before Cubital Tunnel Syndrome Surgery
All surgical procedures incur some risk. However, those specific to ulnar nerve surgery are localized to:
- Wound infection (fortunately the risk for infection is quite low)
- Direct injury to the ulnar nerve
- Persistent or even temporary worsening of symptoms
- Numbness on the posterior aspect of the elbow (due to a small sensory nerve branch separate but overlying the ulnar nerve)
- Recurrent symptoms
Let’s discuss why symptoms would occur again. This is because some patients are genetically more predisposed to developing scar tissue around nerves. Unfortunately, we are not able to identify those who are predisposed to such scaring before surgery. However, the good news is, those of us surgeons seasoned in peripheral nerve surgery are quite familiar with patients exhibiting this phenomenon. In the event this scarring occurs, it may require further surgery. This additional surgery would include concurrent measures with use of different materials to encase the nerve. Alternatively, we can utilize vascularized fat flaps to surround the nerve and limit further scar formation.
What to Expect After Cubital Tunnel Syndrome Treatment
Nerve recovery and symptom resolution varies widely. Some patients note resolution of burning and tingling within just a few days or weeks. For others, depending on the degree and chronicity of nerve compression pre-surgery, this may take a few months. This is particularly the case with patients who demonstrate muscle atrophy changes pre-surgery. Unfortunately, many of those patients will not regain normal muscle function. With this, the goal with nerve compression surgery is to stop the process of ongoing muscle atrophy from lack of neural input. Neural input is in essence, the lack of brain neurons that tell the muscle to function. Fortunately, sensation for less severe cases may recover over a few months. For patients who have had severe or chronic compression, sensation is estimated to take anywhere between six to nine months.
If you are experiencing any symptoms of Cubital Tunnel Syndrome or any other nerve injury, call us today. Our physicians will develop a treatment plan to ensure you do not suffer from any further muscle atrophy and sustain as much normal motor function as possible.
Developed by the Colorado Springs Orthopaedic Group Hand and Upper Extremity Center
Meet Our Providers

Dale Cassidy, MD