What is Frozen Shoulder?
Causes, Symptoms, and Treatment Options
Terms to know:
- Humerus: upper arm bone
- Scapula: shoulder blade
- Clavicle: collarbone
- Shoulder Capsule: group of strong connective tissues that encapsulate and secure the shoulder’s ball and socket joint
- Contracture: when a soft connective tissue around a joint becomes stiff, constricted, or shortened.
- Manipulation under Anesthesia (MUA): when the patient receives general anesthesia and a series of stretching, traction, and mobilization is performed by the surgeon.
- Arthroscopy: a minimally invasive surgical technique that involves using a camera and specially designed instruments that are inserted into the joint via several small incisions.
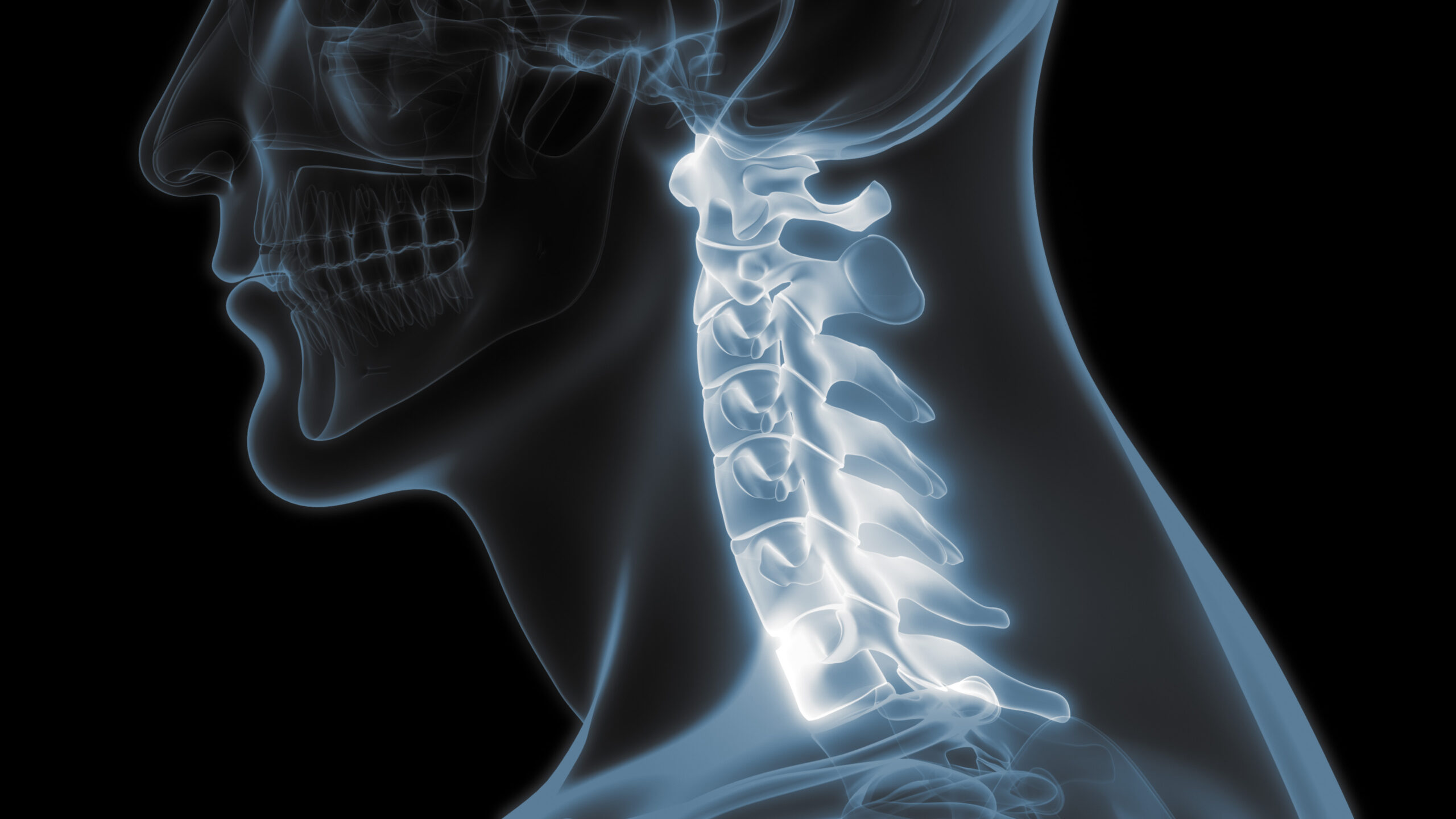
Shoulder Anatomy
The shoulder is a ball-and-socket joint that is made up from three bones: the Humerus (the upper arm bone), the Scapula (commonly known as the shoulder blade), and the Clavicle (collarbone). The humerus fits right into a shallow socket that is formed within the scapula, right under where the clavicle sits above the scapula. Strong connective tissues surround this joint and hold these boney structures in place. These tissues are referred to as the Shoulder Capsule in medical terms. Additionally, Synovial fluid resides within the shoulder capsule and shoulder joint to help the shoulder move with ease.
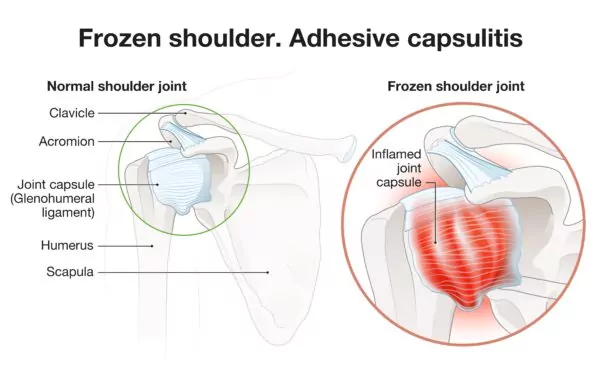
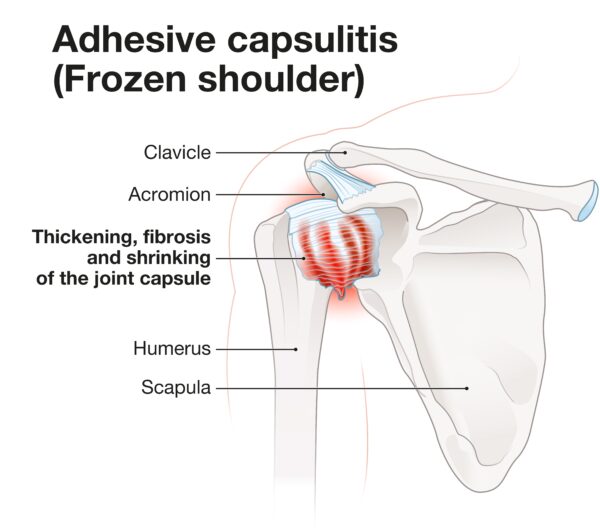
What is Frozen Shoulder?
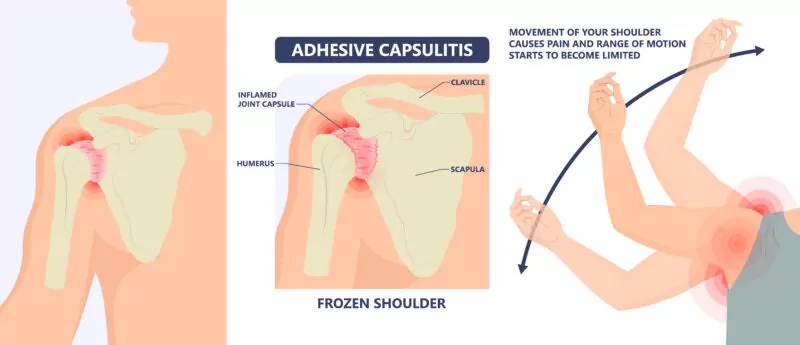
Frozen shoulder, also known as Adhesive Capsulitis, is a condition where the shoulder capsule surrounding the shoulder joint becomes stiff and in turn causes pain in the shoulder. It is a relatively common cause of disabling shoulder pain and dysfunction. Although it is not as common as a rotator cuff problem, the pain it causes is typically much more severe.
Frozen Shoulder Stages
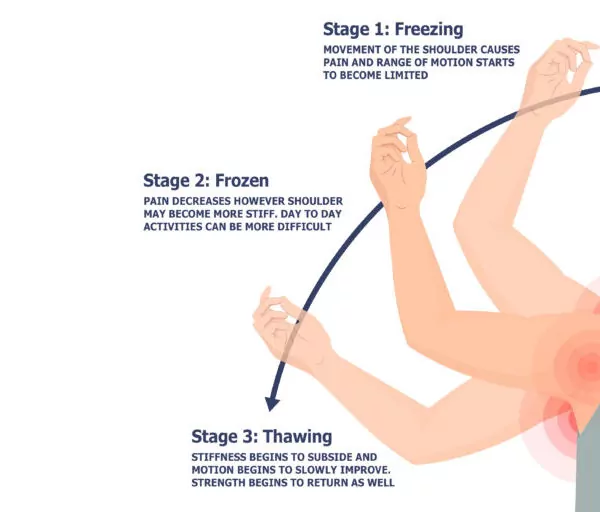
There are three (3) stages of Frozen Shoulder.
Stage one (1) is referred to as the ‘Freezing” stage. This is when pain can worsen and range of motion becomes more limited. This stage typically lasts between six (6) to nine (9) weeks.
Stage two (2) is the ‘Frozen” stage. In many patients, pain may subside to some degree however, stiffness typically remains. Day to day activities can also be very difficult during this stage that can last anywhere between four (4) to six (6) months.
Stage three (3) known as the ‘Thawing’ stage, is when the shoulder stiffness starts to decrease and motions begins to slowly improve. It is within this stage when a patient will begin to return to their normal or close to normal strength as well. This stage is the slowest progression stage and can take anywhere from six (6) months to three (3) years.
What Causes Frozen Shoulder?
Frozen shoulder affects approximately three (3%) percent to five (5%) percent of the general population and tends to affect patients between the ages of forty (40) and sixty (60) years old. The cause of this problem is not well understood however, it involves scarring and contracture of the joint capsule. This scarring and constriction leads to limited mobility of the shoulder joint.
Many who are affected by frozen shoulder do not have any predisposing conditions, however those with diabetes, hypothyroidism or hyperthyroidism, cardiovascular disease, fibrocystic breast disease, or Parkinson’s disease may be more at risk. Additionally, Frozen Shoulder can also develop following trauma to the shoulder, or even after a previous shoulder surgery.
Frozen Shoulder Symptoms
The hallmark physical examination involved with the diagnosis of frozen shoulder is assessing the loss of passive and active mobility in the shoulder joint. Patients often do not acknowledge the significant loss of motion when it occurs as it usually develops slowly and many unconsciously compensate by using more scapular (shoulder blade) motion when performing day to day activities.
Frozen Shoulder Treatment
The good news is that Frozen Shoulder will usually get better without any formal treatment. The bad news is that it can take a very long time (up to several years), and patient symptoms will often trigger them to seek treatment to shorten the course of this problem. To help with this, there are a variety of conservative treatment options available with surgical treatments typically utilized as a last resort for the appropriate patients.
Conservative Treatment Options
Conservative treatments include modalities such as physical therapy for joint mobilizations, oral non-steroidal medications, and steroid injections that can help improve the pain level and restore functional motion. With this, the primary objective in the conservative treatment of frozen shoulder is to control pain while the problem resolves on its own. Studies have shown that, approximately more than ninety percent (90%) of patients see substantial improvements with these various conservative treatments.
Moreover, additional conservative treatment methods have been developed in recent years. These methods however, remain considered as experimental procedures and are not yet approved through the FDA. To learn more about these alternative treatments, we recommend that you further discuss with your physician.
As an alternative to conservative methods if pain and functional limitations are not responding to these conservative treatments, surgery or a Manipulation under Anesthesia can be considered to restore proper mobility. Both conservative and operative treatment methods have shown great success in relieving pain from Adhesive Capsulitis and restoring mobility within the shoulder joint.

Surgical Treatment Options
There are two general operative treatment options to help treat Frozen Shoulder: Manipulation under Anesthesia (MUA) or Arthroscopic Surgery.
Manipulation under Anesthesia
The first, Manipulation under Anesthesia, is performed with the patient completely sedated by an anesthesiologist with intravenous medication. After the patient is asleep, the surgeon simply manipulates the shoulder in a very specific manner to break apart the scar tissue and restore the shoulder’s range of motion. The key to success with this procedure is for the patient to participate in physical therapy and maintain the range of motion after the manipulation.
Arthroscopic Surgery
Secondly, surgery can be performed as an outpatient procedure where the patient will return home the same day as surgery. Typically an Arthroscopic technique is used during this operation. To define, Arthroscopy is a minimally invasive surgical technique that involves using a camera and specially designed instruments that are inserted into the joint via several one quarter inch (1/4”) incisions. The instruments are utilized to cut and remove the scar tissue that is restricting movement. This approach is very effective in restoring normal, or near normal, range of motion. The key with this procedure is that the patient does their part with following their prescribed post-operative physical therapy protocols.
Following surgery of this kind, the arm is kept out of the sling and full range of motion is encouraged from the day of surgery. Daily physical therapy is typically prescribed for the first couple weeks after surgery to help maintain the motion attained during surgery and strengthen the muscles around the joint. This procedure is effective in restoring and maintaining the motion of the shoulder in over ninety (90%) of the cases that require surgery.
If you believe that you are suffering from symptoms of a frozen shoulder, call our office today to schedule with one of our Fellowship Trained Shoulder Specialists. Let’s get you on the road to recovery!
Meet Our Providers

Jamie Friedman, MD

Michael Huang, MD

Christopher Jones, MD

John Redfern, MD

Richard Stockelman, MD