The Link Between BMI and Joint Health: How Weight Impacts Hip and Knee Joint Longevity
As we’ve heard many times before, maintaining a healthy body weight is crucial for overall health, however the impact of a healthy body weight on specific body parts, specifically the hip and knee joints, is often underestimated. Body Mass Index (BMI), a measure of body fat based on height and weight, along with the measure of relative muscle mass, can significantly affect the health and longevity of these weight-bearing joints. Today, we’ll discuss the correlation between BMI and joint health, with focus on the hip and knee joints, and how weight management plays a crucial role in preserving joint function and longevity.
It is important to note, muscle mass has a great influence on BMI measurements as BMI is factored upon height and weight and does not differentiate between muscle mass and fat mass. Muscle tissue is denser than fat tissue, therefore a person with a high muscle mass, but relatively low fat mass may have a higher weight resulting in a higher BMI measurement. This does not necessarily mean that the individual is overweight or unhealthy. The impact of BMI on weight-bearing Joint Longevity discussed within this article, does not pertain to those of high muscle mass with low fat mass measurements.
The Impact of BMI on Hip Joints
The hip joint is one of the largest weight-bearing joints in the body and is responsible for supporting our body weight during both sedentary activities and when facilitating movement. Studies have shown that a higher BMI is associated with an increased risk of hip osteoarthritis, a degenerative joint disease characterized by the breakdown of cartilage and bone within the joint. This is because the excess body weight places additional stress on the hip joint, accelerating the wear and tear process and increasing the risk of developing osteoarthritis. Maintaining a healthy BMI through a nutrient dense diet and consistent exercise regimen can help preserve joint function and longevity.
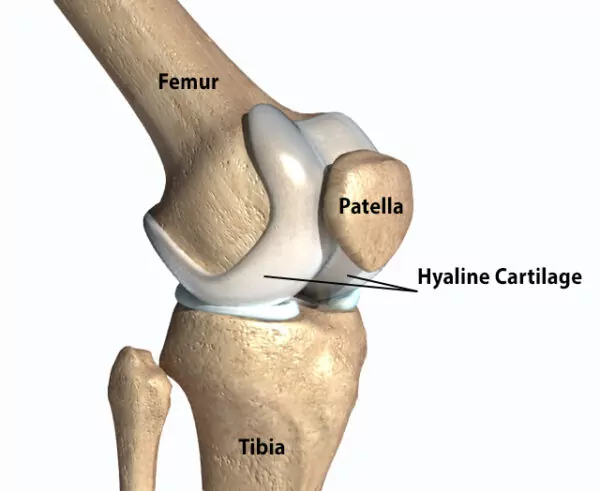
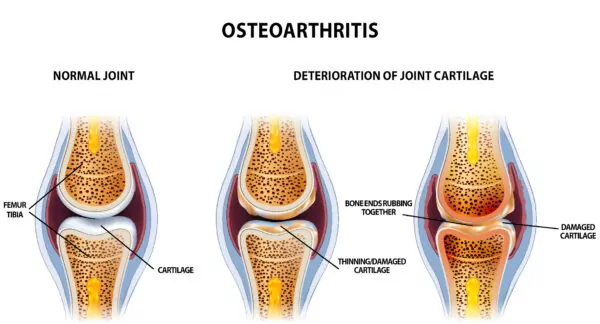
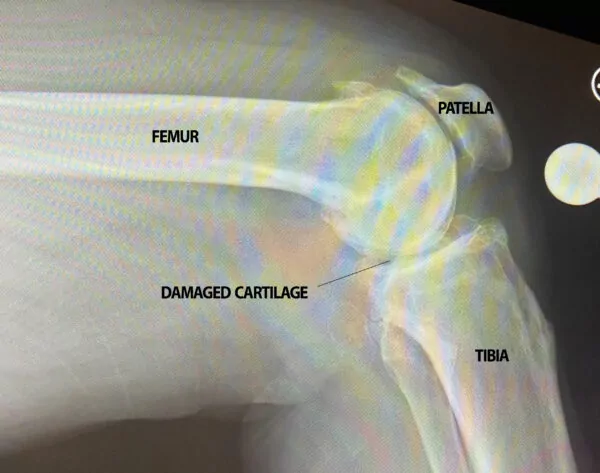
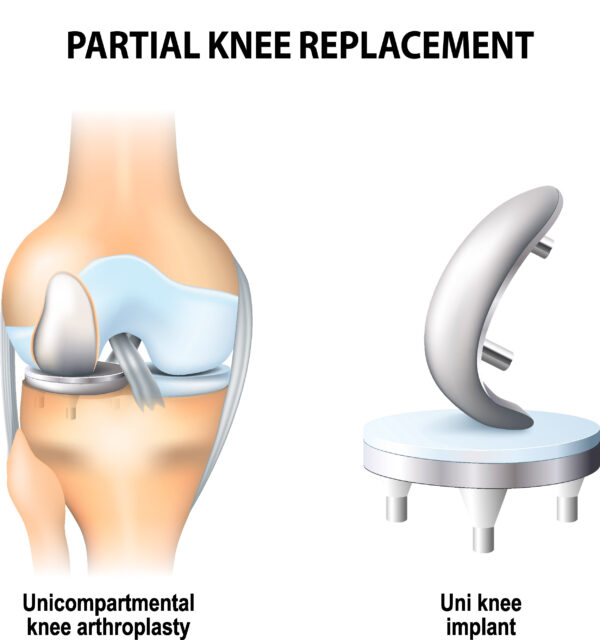
The Effect of BMI on Knee Joints
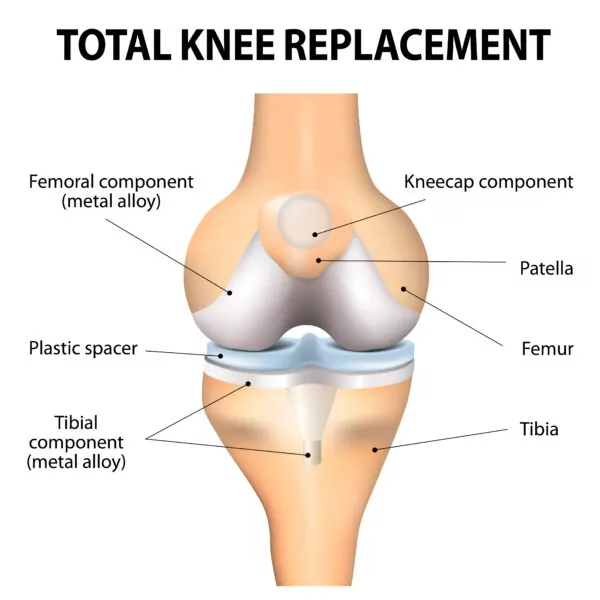
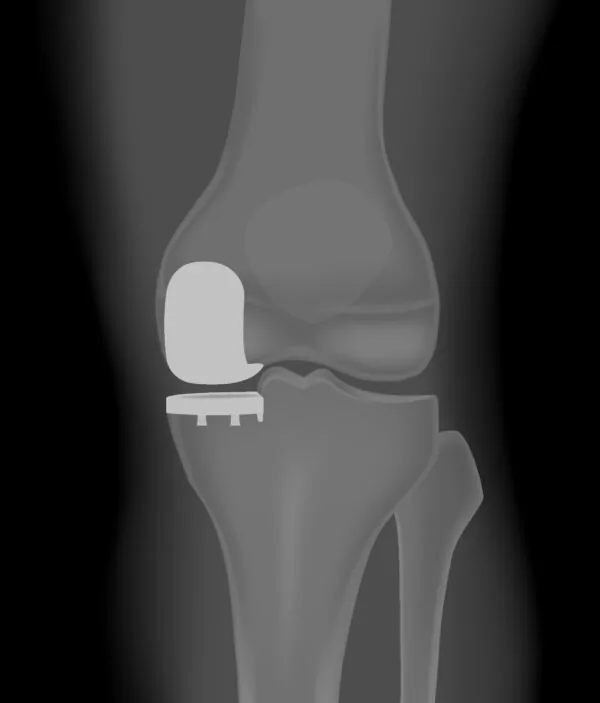
Similar to the hip joint, the knee joint is also susceptible to the effects of excess body weight. Studies have demonstrated a clear link between higher BMI and an increased risk of knee osteoarthritis. The excess weight puts pressure on the knee joint, leading to cartilage damage and inflammation, which are key indicators of osteoarthritis onset. Additionally, higher BMI is associated with an increased risk of knee injuries, such as tears in the ligaments or meniscus, further compromising joint health. By maintaining a healthy BMI, individuals can help protect the integrity of their knee joints, reducing the risk of developing knee osteoarthritis and either delaying the need for a total joint replacement or avoiding one altogether.
The Role of Weight Management in Joint Health
Weight management plays a crucial role in preserving the longevity of the hip and knee joints. For individuals who are overweight or obese, losing even a modest amount of weight can significantly improve joint function.
Maintaining a healthy weight and BMI measurement is especially crucial when looking to qualify for a total joint replacement as BMI is one of the several factors considered when determining a patient’s eligibility for a hip replacement or knee replacement. Although there is not a specific BMI ‘cutoff’ that qualifies or disqualifies a patient, risks such as infections, blood clots, and anesthesia complications, exponentially increase in those with higher BMIs. Generally, a BMI below 40 is preferred as qualification for a total joint replacement to reduce these risks.
The decision to move forward with a hip or knee replacement surgery is inevitably up to the individual and their orthopedic specialist who will complete a comprehensive evaluation of the patient’s overall health, the severity of joint damage, pain during daily activities, and functional limitations. If recommended to reduce one’s BMI measurement, a combination of regular physical activity, such as low-impact exercises like swimming or cycling, or resistance training combined with a nutrient dense diet can help individuals achieve and maintain a healthy BMI, reducing the burden on their joints and maintaining joint health for the long run.
To schedule an appointment with one of our Board Certified and Fellowship Trained specialists, give us a call at 719-632-7669 or visit us at www.CSOG.net to learn more.