Anterior Hip Arthroplasty, Advancing Hip Replacement Outcomes and Longevity
Hip replacement surgery has come a long way since its inception with new techniques continuously evolving to improve outcomes, patient satisfaction, and implant longevity. One such advancement is the use of the anterior approach hip replacement surgery, a technique that differs from traditional approaches (posterior and lateral) and offers many unique benefits. Today, we’ll delve into:
– What Anterior Hip Replacements are
– The History of Anterior Hip Replacements
– How they differ from other techniques
– What recovery generally looks like
– Candidacy for this innovative procedure
What are Anterior Hip Replacements?
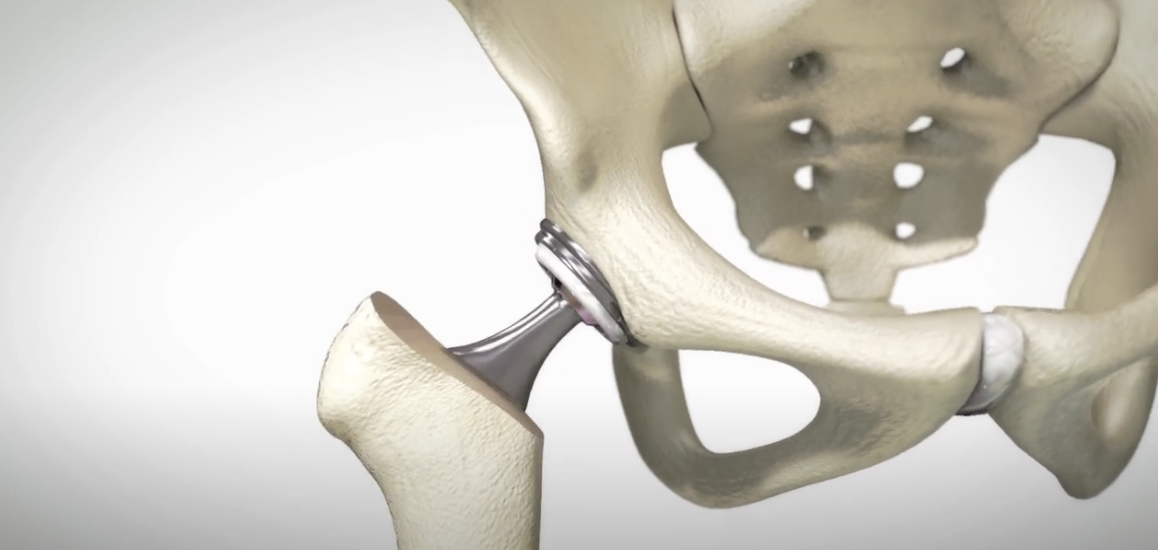
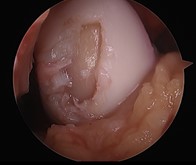
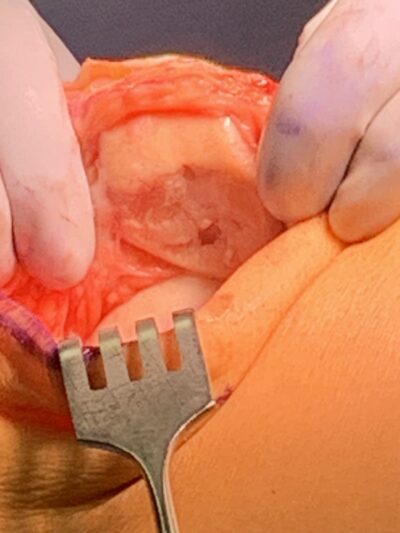
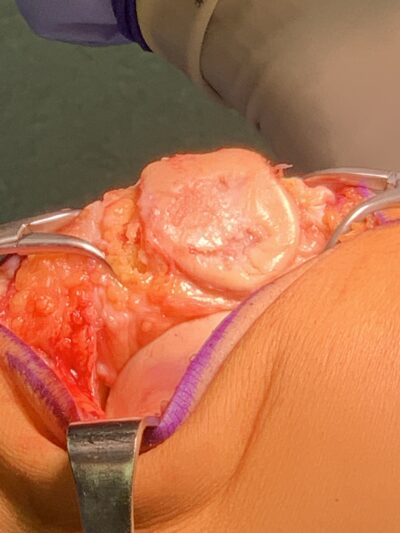
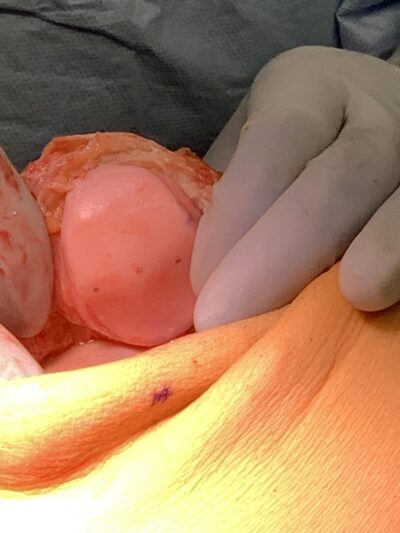
Anterior hip replacement surgery is a minimally invasive surgical technique used to replace a damaged hip joint with an artificial implant. Unlike traditional hip replacement surgeries that access the hip joint from the side or back (lateral or posterior approaches), the anterior approach accesses the joint from the front (anterior aspect) of the hip, through a small incision.
A Brief History
While the anterior approach to hip replacement is often considered a modern innovation, its roots can be traced back to the early 20th century. Dr. Marius Smith-Petersen, an American orthopedic surgeon, first discussed the anterior approach in the 1940s. However, it was not widely adopted due to technological challenges and the popularity of other approaches. The first anterior hip replacement surgery was performed in 1947. It wasn’t until the late 20th and early 21st centuries that advancements in surgical techniques, imaging technology, and implant design made anterior hip replacement a more feasible option. Since these advancements, the procedure has gained immense popularity among surgeons and patients alike.
How Anterior Hip Replacement Differs
The anterior approach offers several advantages over traditional lateral and posterior approach hip replacement techniques including:
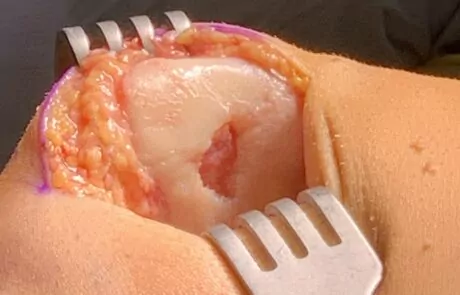
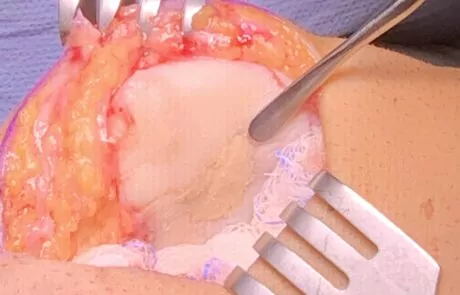
- Muscle Preservation: One of the key benefits of the anterior approach is that it allows access to the hip joint without detaching muscles from the pelvis or femur. A muscle-sparing technique such as this, can lead to faster recovery times and in many cases, less postoperative pain compared to other techniques..
- Stability: Thanks to this muscle preservation, the anterior approach shows an increased stability of the implant due to the preservation of the surrounding soft tissues and muscles. This added stability can reduce the risk of dislocation.
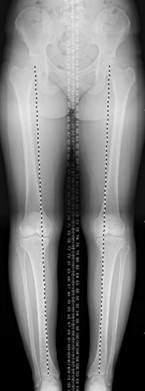
- Additional Accuracy: The anterior approach provides excellent visualization of the hip joint, allowing for even more precise placement of the implant during surgery.
- Faster Recovery: Patients who undergo anterior hip replacement surgery may experience a quicker recovery compared to other techniques. This is primarily due to the muscle preservation benefits, which can lead to less damage to the surrounding structures and a faster return to normal activities.
Video credit to Stryker Orthopedics
Anterior Hip Replacement Recovery
Studies show recovery from Anterior Approach Hip Replacement Surgery enables the potential for:
- Early Mobility: One of the primary advantages of the anterior approach is that it typically allows for early mobility. Patients may be able to walk with a cane or walker soon after surgery, often times within a couple hours of surgery. This is due to the muscle preservation nature of the approach, again, leading to less damage to the surrounding structures and a faster return to normal activities.
- Decreased Postoperative Pain: Because the surgery involves less disruption of muscles and soft tissues, patients undergoing an anterior approach often experience less postoperative pain compared to those undergoing a lateral or posterior approach.
While hip precautions are often recommended for all types of hip replacement surgeries to prevent dislocation of the new hip joint, the specific precautions may vary depending on the surgical approach. For example, patients undergoing an anterior approach may be advised to avoid certain movements that could strain the front of the hip joint especially within the initial recovery period.
Rehabilitation following an anterior approach hip replacement surgery typically focuses on restoring range of motion, strength, and function. To kickstart the recovery process, Physical therapy begins soon after surgery to help patients regain mobility and strength in the hip joint and return to normal activities, including driving, quickly and efficiently.
It’s important to note that the recovery process can vary from patient to patient due to individual factors regardless of the surgical approach. Factors such as age, overall health, and the extent of joint damage can all impact the recovery timelines and overall outcome. Patients should follow their surgeon’s postoperative instructions and participate in any rehabilitation programs as prescribed to optimize their recovery.
Who Would Be a Candidate?
While anterior hip replacement surgery offers many benefits, not everyone is a candidate for this procedure. Ideal candidates for anterior hip replacement surgery typically include those who are:
- Physically Active: Patients who are physically active and in good overall health may benefit from the faster recovery times associated with the anterior approach.
- Of Healthy BMI: Patients who are within a healthy BMI generally have better outcomes with the anterior approach, as excess body weight can put additional stress on the hip joint and may impose greater risk of complications during and after surgery. Tune into our blog discussing The Link between BMI and Joint Health
- Motivated Patients: Patients who are motivated to actively participate in their recovery process, including following postoperative rehabilitation protocols, achieve better results with the anterior approach.
Candidacy for any hip replacement technique ultimately comes down to what is best for the individual patient and their lifestyle as discussed with their orthopedic specialist.
In conclusion, Anterior Hip Arthroplasty surgery is a modern hip replacement technique that offers several advantages. With its muscle preserving technique, increased stability, and faster recovery times, it has become an attractive option for many surgeons and patients seeking hip replacement surgery with hopes of returning to activities.
If you’d like to discuss your candidacy for an anterior hip replacement, give us a call at 719-632-7669 to schedule with one of our board certified Joint Replacement specialists.